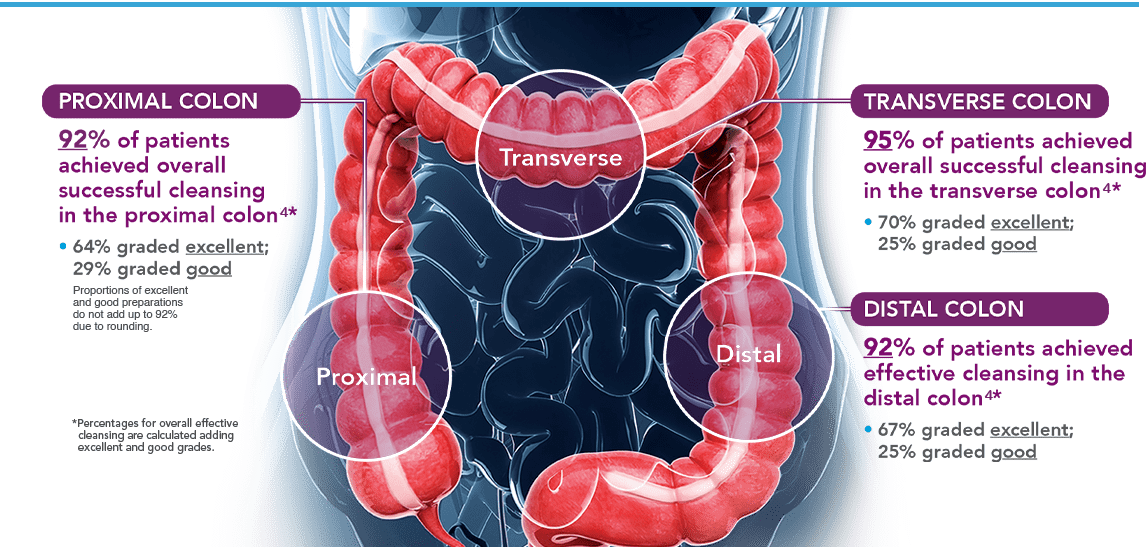
A prep is considered successful if it is good or excellent 2,3
- 97% agreement was seen between central and local readers3
SUTAB® Split-Dose Regimen†
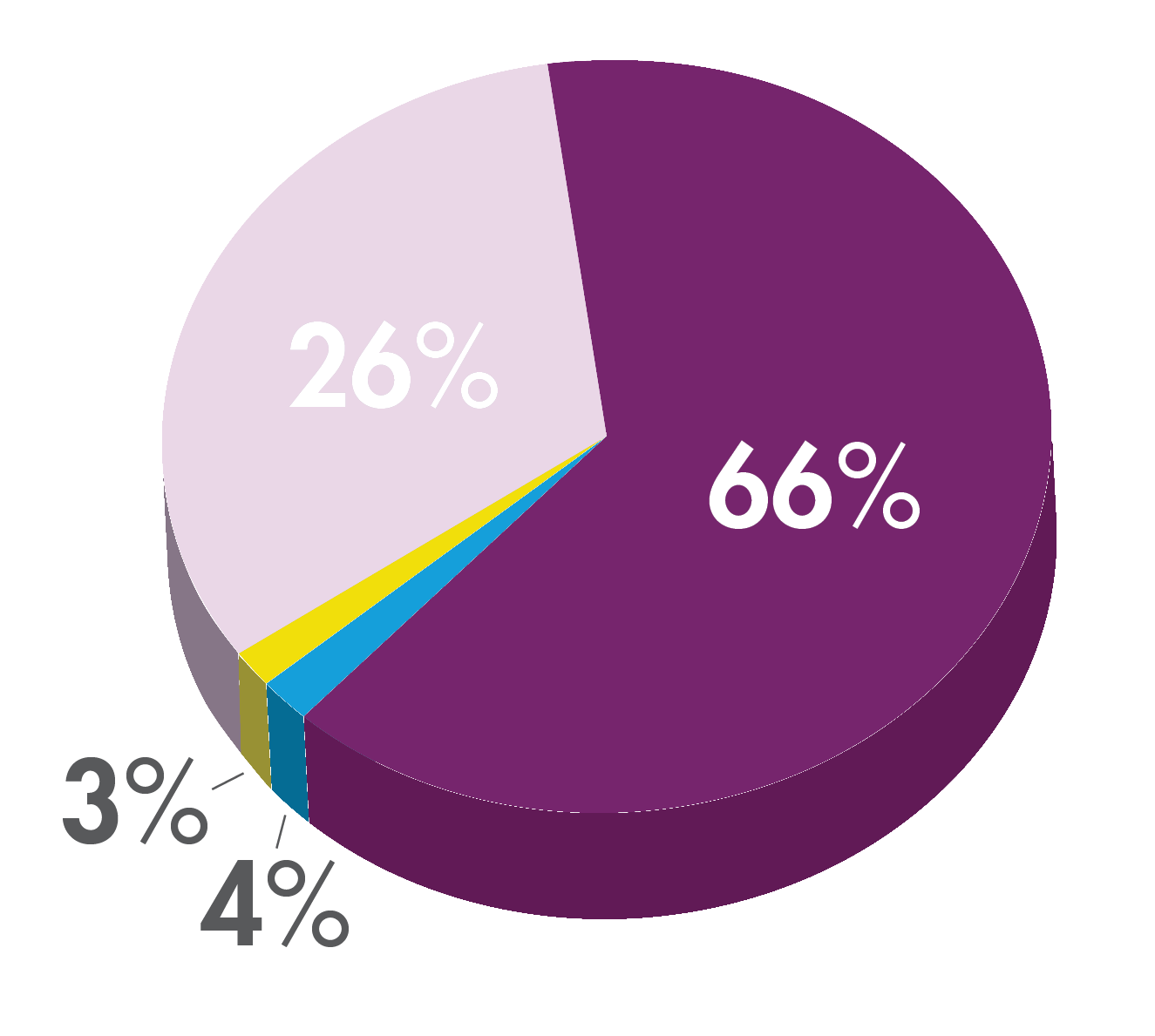
A prep is considered successful if it is good or excellent 2,3
SUTAB® Split-Dose Regimen†
Study Design3: Study 1 was a phase 3 trial that was conducted in 22 US sites. Of the 620 subjects who enrolled, 548 patients were evaluable for efficacy analyses. The primary endpoint was the percentage of subjects with successful cleansing, which was based on the US FDA Bowel Prep Scoring Scale, the goal of which was to determine non-inferiority against MoviPrep®. Safety follow-up visits were required 24-48 hours after colonoscopy and on days 7 and 30 if adverse events or lab abnormalities were indicated. A subset of colonoscopies was graded by central readers (exploratory). The primary endpoint of non-inferiority was met.
| Hard-to-Prep Patients (n=115) | Successful Cleansing Rate |
Excellent Cleansing Rate |
|---|---|---|
|
History of constipation Opioid use Failed colonoscopy BMI ≥35 |
90% | 61% |
| Afternoon colonoscopy (n=49) | 96% | 74% |
| Endpoint | SUTAB Result |
|---|---|
| Cecal intubation rate | 98% |
| Preparation adequacy | 97% |
| Procedure duration (median) | 13.5 minutes |
| Intraprocedural water volume (median) | 30 mL |
Recommended Cecal Intubation Rate: ≥95%
ACG®=American College of Gastroenterology
ASGE®=American Society for Gastrointestinal Endoscopy
INDICATION
SUTAB® (sodium sulfate, magnesium sulfate, potassium chloride) tablets for oral use is an osmotic laxative indicated for cleansing of the colon in preparation for colonoscopy in adults.
CONTRAINDICATIONS
Use is contraindicated in the following conditions: gastrointestinal obstruction or ileus, bowel perforation, toxic colitis or toxic megacolon, gastric retention, hypersensitivity to any ingredient in SUTAB®.
DOSAGE AND ADMINISTRATION
A low residue breakfast may be consumed. After breakfast, only clear liquids may be consumed until after the colonoscopy. Administration of two doses of SUTAB® (24 tablets) are required for a complete preparation for colonoscopy. Twelve (12) tablets are equivalent to one dose. Each SUTAB® bottle contains a desiccant. Remove and discard the desiccant from both bottles the evening prior to the colonoscopy. Water must be consumed with each dose of SUTAB® and additional water must be consumed after each dose. Complete all SUTAB® tablets and required water at least 2 hours before colonoscopy.
WARNINGS AND PRECAUTIONS
Risk of fluid and electrolyte abnormalities: Encourage adequate hydration, assess concurrent medications and consider laboratory assessments prior to and after each use; Cardiac arrhythmias: Consider pre-dose and post-colonoscopy ECGs in patients at increased risk; Seizures: Use caution in patients with a history of seizures and patients at increased risk of seizures, including medications that lower the seizure threshold; Patients with renal impairment or taking concomitant medications that affect renal function: Use caution, ensure adequate hydration and consider laboratory testing; Colonic mucosal ulcerations: Consider potential for mucosal ulcerations when interpreting colonoscopy findings in patients with known or suspected inflammatory bowel disease. Suspected GI obstruction or perforation: Rule out the diagnosis before administration. Hypersensitivity reactions, including anaphylaxis: Inform patients to seek immediate medical care if symptoms occur. Risk of Gastrointestinal Complications with Ingestion of Desiccant: Postmarketing reports of ingestion of the desiccant along with SUTAB® tablets has been reported and may be associated with risk of gastrointestinal complications and/or choking.
ADVERSE REACTIONS
Most common gastrointestinal adverse reactions are: nausea, abdominal distension, vomiting, and upper abdominal pain.
DRUG INTERACTIONS
Drugs that increase risk of fluid and electrolyte imbalance.
View the Full Prescribing Information and Medication Guide.
References: 1. IQVIA, National Prescription Audit Report. December 2023. 2. SUTAB® [package insert]. Braintree, MA: Braintree Laboratories, Inc. 3. Di Palma JA, Bhandari R, Cleveland M, et al. A safety and efficacy comparison of a new sulfate-based tablet bowel preparation versus a PEG and ascorbate comparator in adult subjects undergoing colonoscopy. Am J Gastroenterol. 2021;116(2):319-328. doi: 10.14309/ajg.0000000000001020. 4. Rex DK, Johnson DA, Anderson JC, et al; American College of Gastroenterology. American College of Gastroenterology guidelines for colorectal cancer screening 2009 [corrected]. Am J Gastroenterol. 2009;104(3):739-750. 5. Rex DK, Boland CR, Dominitz JA, et al. Colorectal cancer screening: recommendations for physicians and patients from the US Multi-Society Task Force on Colorectal Cancer. Am J Gastroenterol. 2017;112(7):1016-1030. doi:10.1038/ajg.2017.174. 6. Rex DK, Anderson JC, Butterfly LF, et al. Quality indicators for colonoscopy. Gastrointest Endosc. 2024;100(3):352-381. doi:10.1016/j.gie.2024.04.2905 7. Data on file. Braintree Laboratories, Inc. Braintree, MA. 8. SUFLAVE™ [package insert]. Braintree, MA: Braintree Laboratories, Inc. 9. SUPREP® Bowel Prep Kit [package insert]. Braintree, MA: Braintree Laboratories, Inc. 10. Plenvu® [package insert]. Bridgewater, NJ: Bausch Health LLC. 11. Clenpiq® [package insert]. Parsippany, NJ: Ferring Pharmaceuticals, Inc. 12. Rex DK, Di Palma JA, Rodriguez R, et al. A randomized clinical study comparing reduced-volume oral sulfate solution with standard 4-liter sulfate-free electrolyte lavage solution as preparation for colonoscopy. Gastrointest Endosc. 2010;72(2):328-336. 13. Matro R, Daskalakis C, Negoianu D, et al. Randomised clinical trial: polyethylene glycol 3350 with sports drink vs polyethylene glycol with electrolyte solution as purgatives for colonoscopy—the incidence of hyponatraemia. Aliment Pharmacol Ther. 2014;40(6):610-619.
SUFLAVE™ (polyethylene glycol 3350, sodium sulfate, potassium chloride, magnesium sulfate, and sodium chloride for oral solution) is an osmotic laxative indicated for cleansing of the colon in preparation for colonoscopy in adults.
DOSAGE AND ADMINISTRATIONA low residue breakfast may be consumed on the day before colonoscopy, followed by clear liquids up to 2 hours prior to colonoscopy. Administration of two doses of SUFLAVE™ are required for a complete preparation for colonoscopy. Each bottle must be reconstituted with water before ingestion. Each bottle and one flavor enhancing packet are equivalent to one dose. An additional 16 ounces of water must be consumed after each dose. Stop consumption of all fluids at least 2 hours before the colonoscopy.
CONTRAINDICATIONSUse is contraindicated in the following conditions: gastrointestinal obstruction or ileus, bowel perforation, toxic colitis or toxic megacolon, gastric retention, hypersensitivity to any ingredient in SUFLAVE™.
WARNINGS AND PRECAUTIONS
Risk of fluid and electrolyte abnormalities: Encourage adequate hydration,
assess concurrent medications and consider laboratory assessments prior to and after each use; Cardiac arrhythmias: Consider pre-dose and
Most common adverse reactions (≥2%) are: nausea, abdominal distension, vomiting, abdominal pain, and headache.
DRUG INTERACTIONSDrugs that increase risk of fluid and electrolyte imbalance.